continuous trend monitoring
the new standard of care
introduction
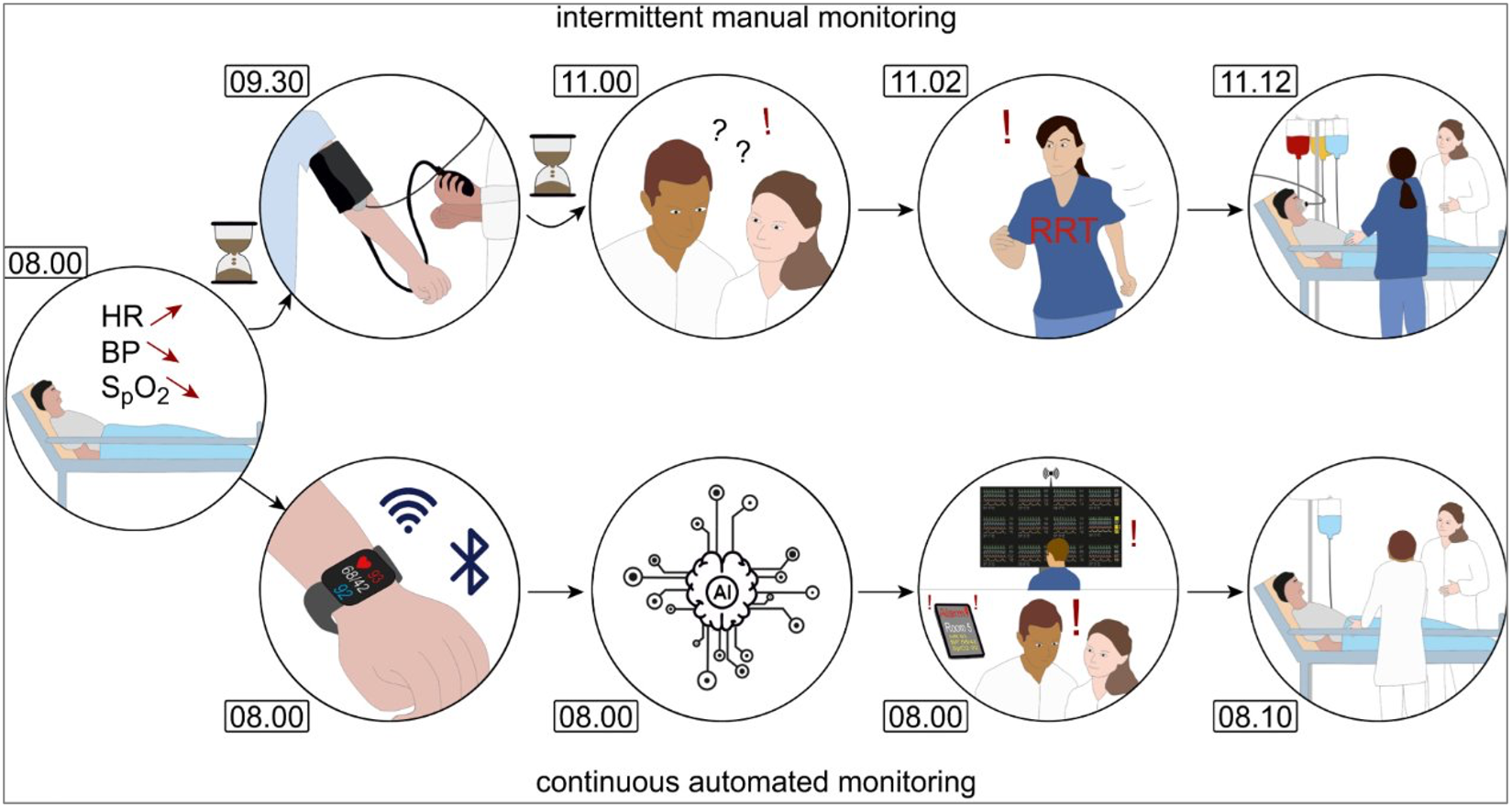
Monitoring vital signs is crucial for the timely detection of deterioration, complications and improved clinical outcomes. Traditionally, vital signs in clinical settings have been measured intermittently and manually according to standardized protocols—a method known as Intermittent Monitoring (IM). While this approach has been effective, its limitations have become more apparent with the emergence of Continuous Trend Monitoring (CM). These shortcomings include missed early warning signs of deterioration, leading to complications and a high workload for healthcare professionals.
With the advent of wireless technologies, CM has become increasingly accessible. This technology enables real-time continuous data collection, allowing healthcare providers to detect changes in vital signs before they escalate into critical situations. To successfully implement CM as the new standard of care, it is essential to focus on key aspects such as technical integration with existing systems and adjustments to clinical protocols. These protocols should define how to monitor trends and determine the appropriate response strategies.
Additionally, clinical trainings are necessary to emphasize the importance of trend analysis over reliance on absolute values, which can be temporary and variable in intermittent measurements.
In this whitepaper, we compare CM with IM and discuss the benefits of trend monitoring based on recent studies. Additionally, we identify the key factors required for the successful implementation of CM and its adoption as the new standard of care.
continuous trend monitoring vs. intermittent monitoring
When comparing continuous trend monitoring (CM) with intermittent monitoring (IM), key differences emerge in their impact on patient care, healthcare efficiency, and clinical outcomes. The following sections explore these aspects in detail.
- Early Detection of Clinical Deterioration
Continuous Trend monitoring (CM) enables the early identification of subtle changes in vital signs compared to IM [3,4,5,6]. Studies indicate that CM detects significant abnormalities an average of 42.8 hours earlier than IM, allowing for faster intervention and potentially reducing mortality and ICU admissions [2,3,9]. - Reduced Workload and Time Savings for Healthcare Professionals
A study conducted in Denmark demonstrated that CM significantly reduced the time spent on vital sign monitoring, from 480 minutes per day for all patients on one general ward with IM to just 113 minutes with CM. This translates to a median time reduction from 14 to 6 minutes per patient per day (p<0.001)[10]. These findings suggest that CM can alleviate the workload for healthcare professionals, allowing them to dedicate more time to direct patient care. - Impact on Patient Outcomes
Prospective cohort studies have shown that CM is associated with a reduced risk of ICU admissions and in-hospital mortality. Patients monitored continuously had a lower risk of heart failure (Odds Ratio (OR) 1.48) and myocardial infarction (OR 3.87) compared to those monitored intermittently [9].
successful integration and adoption of continuous trend monitoring (CM) in clinical practice
While CM offers significant advantages, several key factors influence its successful implementation and widespread adoption in clinical practice:
technical integration and infrastructure
Seamless integration of CM systems with existing hospital infrastructure is crucial. This includes reliable connectivity and compatibility with Electronic Health Records (EHRs) to ensure real-time access to vital parameters for healthcare providers. Additionally, it eliminates the need for caregivers to log into multiple systems, promoting easier adoption. Solutions such as viQtor and Healthdot, which are wearable sensors designed to measure vital functions such as heart rate, respiratory rate, and oxygen saturation in patients, demonstrate the potential for effective integration with existing EHRs. By continuously monitoring these parameters, these devices help detect early signs of patient deterioration, enabling timely interventions. This integration is a critical step in the successful adoption of continuous monitoring (CM) [4,7,11].
workflow optimization and clinical decision-making
Transitioning from IM to CM requires a revision of current clinical protocols. Rather than relying on periodic absolute values, healthcare providers must be trained in interpreting trends and implementing appropriate interventions when these trends are changing. Additionally, they will need guidance on how to set and handle notifications for trend changes. Successful implementation demands multidisciplinary collaboration between nurses and physicians, integrating trend monitoring into clinical decision-making [4, 6,7,11].
Additionally, clinical innovators within healthcare teams are needed to drive the acceptance of CM technology. Through proactive guidance and positive experiences, these innovators can facilitate the transition to CM and accelerate adoption. Effective workflow integration is essential for broader acceptance and long-term sustainability.
managing notifications fatigue
Excessive false notifications can lead to notifications fatigue among healthcare staff, hindering the acceptance and effectiveness of CM systems. Unlike IM, where vital signs are checked at fixed intervals, CM continuously tracks physiological trends. To ensure meaningful and actionable notifications, these should only be triggered when a threshold value is exceeded for a prolonged period, rather than reacting to brief fluctuations.
To mitigate this, hospitals should implement Early Warning Score (EWS) protocols specifically tailored to CM and the patient population admitted to their department. These protocols should customize threshold values based on the patient’s condition or clinical status. Additionally, introducing time-weighted notification mechanisms can help reduce unnecessary notifications. This ensures that critical warnings are delivered in a timely and reliable manner. This approach allows healthcare providers to focus on clinically significant deteriorations rather than transient changes, improving overall patient safety and workflow efficiency [van Noordt et al].
Additionally, in some cases, although no automated notifications are used, healthcare providers may review patient data more frequently than the standard three times per day to detect early signs of deterioration in physiological trends. This proactive approach aims to identify issues sooner, even without continuous notifications.
conclusion
Continuous Trend monitoring (CM) offers significant advantages over intermittent monitoring (IM), particularly in early detection of deterioration, leading to reducing complications and ICU admissions, and reducing healthcare workload. However, successful implementation requires careful consideration of technological integration, workflow optimization, and notification management to ensure adoption in clinical practice.
recommendations
- Seamless integration of CM systems with existing hospital EPDs to streamline workflows, eliminating the need for separate logins and will reduce the workload for healthcare professionals.
- Comprehensive training and adoption programs for healthcare staff to facilitate CM implementation. These programs should include training on interpreting trends, managing notifications, and addressing change management processes to ensure a smooth transition and effective use in CM technology.
- Development of trend monitoring protocols to standardize clinical response strategies.
References:
- Becking-Verhaar, F. L., Verweij, R. P. H., de Vries, M., Vermeulen, H., van Goor, H., & Huisman-de Waal, G. J. (2023). Continuous Vital Signs Monitoring with a Wireless Device on a General Ward: A Survey to Explore Nurses’ Experiences in a Post-Implementation Period. International Journal of Environmental Research and Public Health, 20(10), 5794. https://doi.org/10.3390/ijerph20105794
- Eddahchouri, Y., Peelen, R. V., & Touw, H. (2023). The Effect of Continuous Versus Periodic Vital Sign Monitoring on Disease Severity of Patients with an Unplanned ICU Transfer. Journal of Medical Systems, 47, 43. https://doi.org/10.1007/s10916-023-01943-2
- Jensen, M. S. V., Eriksen, V. R., Rasmussen, S. S., Meyhoff, C. S., & Aasvang, E. K. (2024). Time to Detection of Serious Adverse Events by Continuous Vital Sign Monitoring Versus Clinical Practice. Acta Anaesthesiologica Scandinavica, 69(1), e14541. https://doi.org/10.1111/aas.14541
- Khanna, A. K., Flick, M., & Saugel, B. (2024). Continuous Vital Sign Monitoring of Patients Recovering from Surgery on General Wards: A Narrative Review. Journal of Clinical Monitoring and Computing. Advance online publication. https://doi.org/10.1007/s10877-024-00987-1
- Khanna, A. K., Banga, A., Rigdon, J., White, B. N., Cuvillier, C., Ferraz, J., Olsen, F., Hackett, L., Bansal, V., & Kaw, R. (2023). Role of Continuous Pulse Oximetry and Capnography Monitoring in the Prevention of Postoperative Respiratory Failure, Postoperative Opioid-Induced Respiratory Depression and Adverse Outcomes on Hospital Wards: A Systematic Review and Meta-Analysis. Anesthesia & Analgesia. https://doi.org/10.1213/ANE.0000000000006743
- Leenen, J. P. L., Schoonhoven, L., & Patijn, G. A. (2024). Wearable Wireless Continuous Vital Signs Monitoring on the General Ward. Current Opinion in Critical Care, 30(3), 275-282. https://doi.org/10.1097/MCC.0000000000001160
- Leenen, J. P. L., Dijkman, E. M., van Hout, A., Kalkman, C. J., Schoonhoven, L., & Patijn, G. A. (2022). Nurses’ Experiences with Continuous Vital Sign Monitoring on the General Surgical Ward: A Qualitative Study Based on the Behaviour Change Wheel. BMC Nursing, 21, Article 60. https://doi.org/10.1186/s12912-022-00820-1
- Leenen, J. P. L., Rasing, H. J. M., van Dijk, J. D., Kalkman, C. J., Schoonhoven, L., & Patijn, G. A. (2022). Feasibility of Wireless Continuous Monitoring of Vital Signs Without Using Alarms on a General Surgical Ward: A Mixed Methods Study. PLOS ONE. https://doi.org/10.1371/journal.pone.0265435
- Rowland, B. A., Motamedi, V., Michard, F., Saha, A. K., & Khanna, A. K. (jaar). Impact of continuous and wireless monitoring of vital signs on clinical outcomes: A propensity-matched observational study of surgical ward patients. Tijdschriftnaam, volume(issue), paginabereik. https://doi.org/*DOI*
- Sigvardt, E., Grønbæk, K. K., Jepsen, M. L., Søgaard, M., Haahr, L., Inácio, A., Aasvang, E. K., & Meyhoff, C. S. (2023). Workload Associated with Manual Assessment of Vital Signs Compared with Continuous Wireless Monitoring. Acta Anaesthesiologica Scandinavica, 68(2), 274-279. https://doi.org/10.1111/aas.14333
- van Noort, H. H. J., Becking-Verhaar, F. L., Bahlman-van Ooijen, W., Pel, M., van Goor, H., & Huisman-de Waal, G. (2024). Three Years of Continuous Vital Signs Monitoring on the General Surgical Ward: Is It Sustainable? A Qualitative Study. Journal of Clinical Medicine, 13(2), 439. https://doi.org/10.3390/jcm13020439
- Yadav, A., Dandu, H., Parchani, G., Chokalingam, K., Kadambi, P., Mishra, R., Jahan, A., Teboul, J. L., & Latour, J. M. (2024). Early Detection of Deteriorating Patients in General Wards Through Continuous Contactless Vital Signs Monitoring. Frontiers in Medical Technology, 6. https://doi.org/10.3389/fmed.2024.1436034